Breast Reconstruction Revision
In Beverly Hills, CA
Our Beverly Hills breast reconstruction specialists are highly respected leaders in the field of breast reconstruction revision. Highly sought after by women to correct breast reconstruction surgery performed by other surgeons. Using advanced techniques honed from over 20 years of experience, they artfully and correct the breast shape and position to give women a natural-looking and more natural feeling breast. With decades of experience, Dr. Cassileth and Dr. Killeen have mastered advanced breast reconstruction and revision techniques, offering patients unparalleled expertise and renewed confidence.
Breast Reconstruction Revision at a Glance
- Breast reconstruction revision corrects asymmetry, discomfort, an unnatural-looking result, and implant malposition
- Techniques include implant replacement with fat grafting, repositioning of implants, and correction of capsular contracture.
- Each surgery is uniquely tailored to the patient’s needs and goals.
- Detection of potential biofilms
Breast reconstruction revision procedures focus on correcting and improving the results of a previous breast reconstruction procedure. Depending on your desires, breast reconstruction revision may involve removing or replacing implants, creating a more natural or proportionate appearance, or re-sculpting the breasts to correct abnormalities in the breasts’ shape.

1 of 9
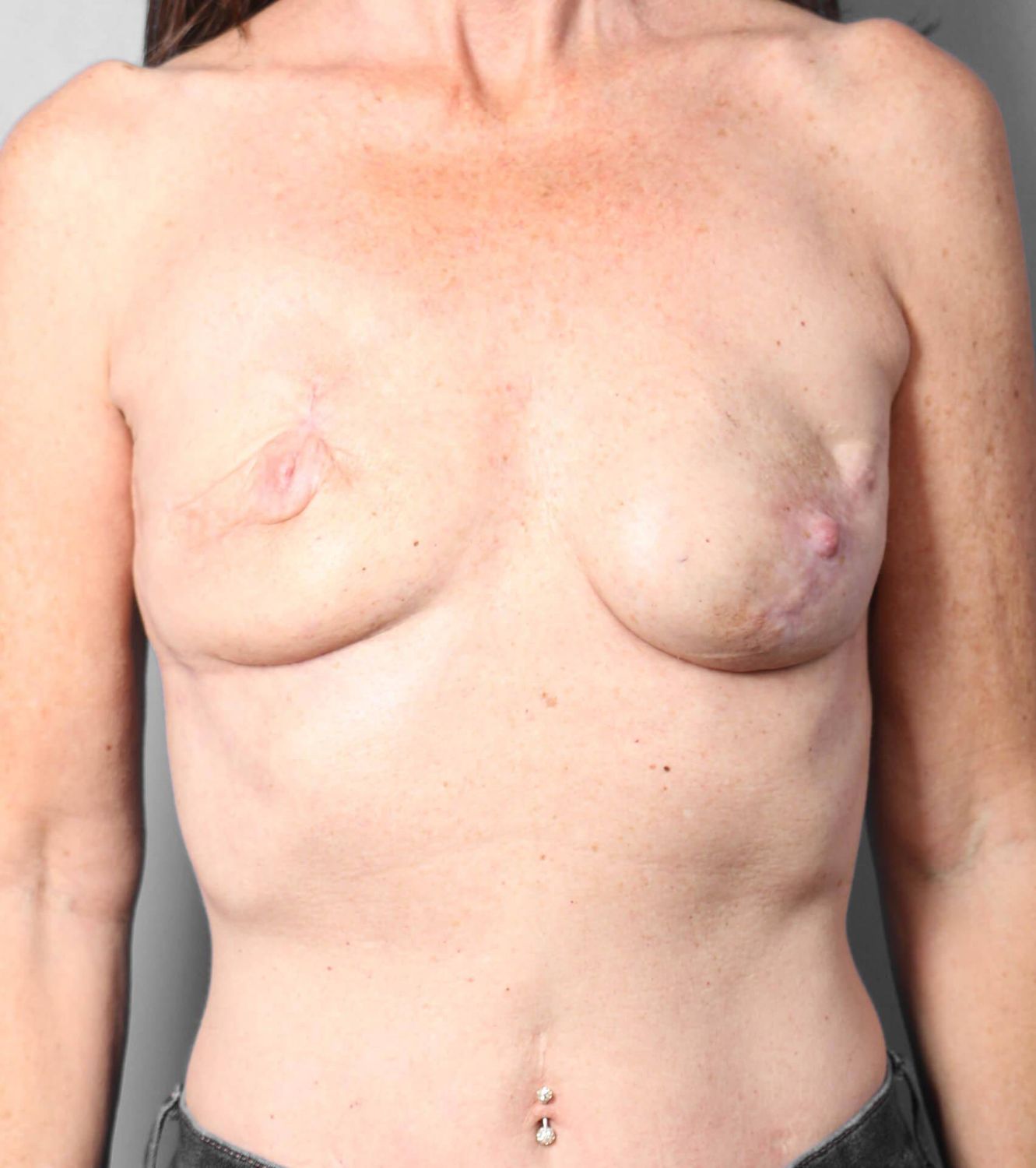
Reconstruction Revision Before & Afters
Common issues following breast reconstruction that lead people to have a revision include breast asymmetry, capsular contracture, implant malposition, or the need or desire to change the size or shape of the implants, or have them removed completely.

After undergoing a unilateral mastectomy, patients may find that one breast sits too high on the chest wall compared to the other breast. Our surgeons use a range of techniques to provide a more balanced, natural appearance. These methods focus on adjusting the soft tissue in the reconstructed breast to create a more natural appearance while enhancing the contour and position.
Autologous fat transfer, which uses fat from another part of the body, adds softness around the reconstructed breast and provides a smooth transition from the implant to the chest wall. Meanwhile, we recontour the unreconstructed breast with methods like a breast lift or implant augmentation to provide a more natural appearance and improved symmetry between the breasts. For patients who don’t want an implant placed in the natural breast, our surgeons may use other advanced techniques to enhance this breast’s lift and volume.
Capsular contracture is a common complication of breast implant surgery. It occurs when the normally thin capsule of scar tissue that naturally forms around the implant thickens and hardens. This can cause the breasts to become firm, rise to a higher position on the chest, and lead to chronic pain and discomfort. To address capsular contracture, we perform a procedure called a capsulectomy. The breast implant is removed and the layer of scar tissue around the implant is completely excised.
Our surgeons support the breast implant with with acellular dermal matrix or absorbable mesh that is placed in the breast pocket. The matrix helps hold the implant in an optimal position while minimizing the recurrence of capsular scar tissue. This additional support allows the breast implant to sit in the correct position and minimizes the chances of forming new scar tissue following breast reconstruction revision surgery. Fat grafting may also be used to improve the shape and softness of the breast.
Without the proper support, a breast implant placed during unilateral breast reconstruction can shift from the original position, causing the implant to become visible or feel heavy on the chest. Bilateral implant patients may have too much distance between their breasts, resulting in a hollow appearance in the upper area of the chest or implant rippling.
The solution is to create a support structure for the implant that acts like an internal bra. In most cases, our material of choice for adding support is an absorbable mesh. Unlike an acellular dermal matrix, which is sometimes used for this purpose, the absorbable mesh resists the tendency to stretch out. Cohesive gel implants (commonly referred to as “gummy bear” implants because of their consistency) are often used because they minimize the risk of rippling. Finally, we use fat transfer to build soft volume between and above the breasts, providing a smooth transition around the implants and correcting a too-wide cleavage gap.

Mastectomy patients who no longer want breast implants may be candidates for removal of the implants, with the volume replaced through fat grafting breast augmentation. Our staged approach involves gradually reducing the size of the implant and replacing the volume with fat from the abdomen, lower back, legs, or arms. The final outcome is the complete removal of the implant, which is replaced with the grafted fat.
Patients who have larger implants will first have their implants replaced by a tissue expander. Fat is then grafted to add volume to the mastectomy flap. The tissue expander is reduced in a series of mini-surgeries until it can finally be removed.
Replacing smaller implants with fat grafts is typically a shorter process. In the first surgery, the size of the implant is decreased and partially replaced with fat. In the second surgery, more fat is added and the implant size can be decreased again, or implants removed.
Most patients require between two and four surgeries, depending on factors like the size of their breast implants and the amount of fat available for harvest in another body area. For patients whose implants are in the submuscular position, the surgeon will also need to repair the pectoral muscles. Patients who have undergone radiation treatment are good candidates for implant replacement with fat grafts. Because the donor fat has not undergone radiation, it helps restore a natural look and feel to the radiated breast.

The consultation phase is very important to the entire surgical process. At your first meeting with your plastic surgeon, you will have the chance to talk about your concerns with your reconstructed breasts and the look and feel you want to achieve with your reconstruction revision surgery. Your surgeon will answer your questions and help you understand all of your surgical options, weighing the pros and cons of different approaches. The consultation also includes a review of your medical history and a breast exam. Finally, your surgeon will design a treatment plan that is tailored to your medical needs and specific aesthetic goals.
Pre-operative preparations may include stopping the use of certain medications. Smokers must quit smoking several weeks before surgery. You will receive detailed instructions on preparing for surgery to ensure a safe procedure. On the day of surgery, general anesthesia will be administered. Each surgery is unique to your needs. Your surgeon will go over specific techniques that will be used in your breast reconstruction revision during pre-operative planning. We strongly emphasize patient education so that you know exactly what to expect as you prepare for your procedure.
Breast reconstruction revision surgery can be a significant step in helping you achieve a sense of closure following your journey with breast cancer. Achieving a more natural-looking and aesthetically pleasing breast appearance can provide a significant boost in self-confidence, as well as impart a sense of wholeness to women who have undergone a mastectomy. Revision surgery also alleviates any physical pain or discomfort resulting from a previous revision surgery. Our highly skilled surgeons are dedicated to restoring patients’ physical and emotional well-being through our expert breast reconstruction revision techniques.
Like pre-operative preparation, recovery is a very important stage of your breast revision journey. Your surgeon will provide you with detailed aftercare instructions and check your healing progress at post-operative appointments. The first few days after surgery are when swelling and discomfort tend to peak. Getting plenty of rest during this time is important. Patients are cleared for a gradual return to more strenuous activities over the next several weeks.
As postoperative swelling fades, your results will become more refined. Our patients tend to be very satisfied with their choice to undergo breast reconstruction revision with our specialists. At this time, you can enjoy a more natural, shapely, and symmetrical breast profile, renewed comfort in your body, and renewed confidence in your appearance. Breast reconstruction revision is an excellent way to achieve a sense of closure and success at the end of your mastectomy journey.

Some of the most common reasons for seeking breast reconstruction revision are implants that are visible, malpositioned or displaced implants, implant rupture, capsular contracture, implant rippling, breast asymmetry, skin or nipple malposition, skin laxity, or dissatisfaction with the result of a previous reconstruction.
This depends on various individual factors. To allow time for healing, we recommend patients wait a minimum of six months after their initial breast reconstruction surgery. Revision may be sought earlier if there is a complication that needs immediate attention.
Elective revision surgery that is primarily cosmetic in nature may not be covered. Insurance may cover revision surgery that is considered medically necessary. Coverage will depend on the specifics of your insurance plan.